Many women experience subtle changes in their bodies that they brush off as “normal” aging, stress, or hormonal shifts. But sometimes, these changes can signal that something more serious is happening with your uterus. Abnormal vaginal bleeding, pelvic discomfort, and other unusual signs often go unnoticed until they become persistent – and by then, early intervention might have made a big difference. The good news? Listening to your body and talking to a healthcare provider about any concerning symptoms can lead to timely evaluation. In this article, we’ll explore 12 key warning signs that deserve attention, based on insights from reputable sources like the American Cancer Society and Mayo Clinic. Stay with me until the end – there’s an important step you can take right now to protect your health that many women overlook.
Why These Signs Matter More Than You Think
Your uterus is an incredible organ that works hard every month, but when something disrupts its normal function, it often sends signals through bleeding patterns, pain, or other changes. Research shows that paying attention to these clues can help identify issues early, when they’re often more manageable. But here’s the truth: most of these symptoms have common, non-serious causes too – like fibroids, hormonal imbalances, or polyps. That’s why it’s never about jumping to conclusions, but about being proactive.
But that’s not all… let’s dive into the specific signs women commonly report but too often ignore.

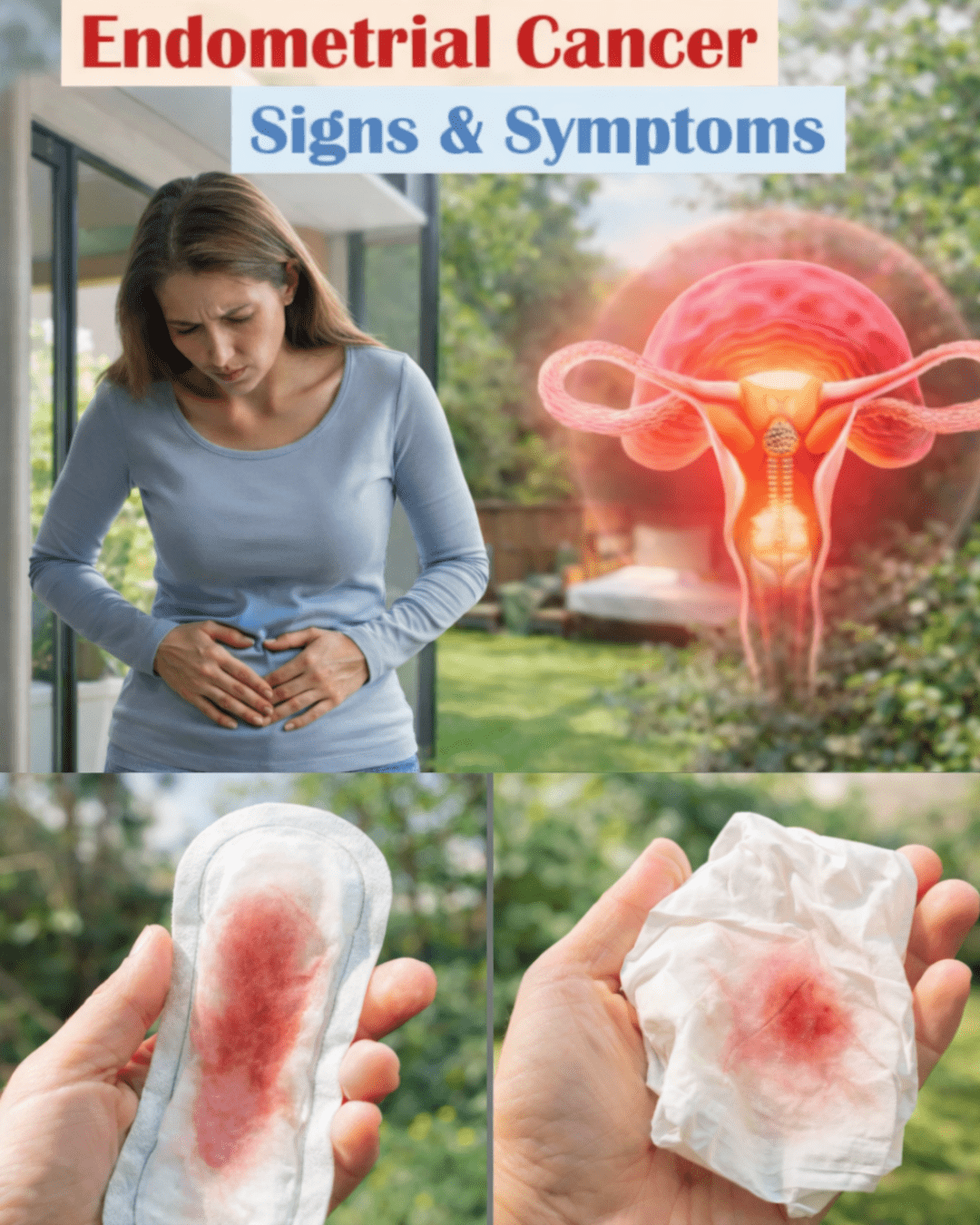
1. Abnormal Vaginal Bleeding – The Most Common Red Flag
Abnormal vaginal bleeding tops the list for a reason. This includes:
- Bleeding between regular periods
- Heavier or longer periods than usual
- Spotting or bleeding after sex
- Any vaginal bleeding after menopause (even a small amount)
Studies from organizations like the American Cancer Society emphasize that this is the most frequent sign linked to endometrial concerns. If you’re postmenopausal and see any spotting, don’t wait – it’s especially important to get checked.
2. Unusual Vaginal Discharge
Not all discharge is cause for alarm, but watch for watery, pink-tinged, or foul-smelling discharge that isn’t related to your cycle. Even if there’s no visible blood, this can be a subtle hint that something needs evaluation.
3. Pelvic Pain or Pressure
A constant feeling of fullness, aching, or pressure in your lower abdomen or pelvis – especially if it’s new or worsening – shouldn’t be dismissed as “just cramps.” This discomfort can feel like a heavy weight or sharp twinges.

4. Pain During Intercourse
If intimacy suddenly becomes painful (known as dyspareunia), it could point to changes affecting the uterus or surrounding tissues. Many women describe this as deep pelvic soreness.
5. Changes in Menstrual Cycle Patterns
Irregular cycles, missed periods (not due to pregnancy or birth control), or dramatically different flow can signal imbalances that warrant a closer look.
6. Unexplained Weight Loss
Losing weight without trying, especially alongside other symptoms, is something to note. In later stages, this can occur, but early detection focuses on the earlier signs.
Here are more signs to watch for in a quick list:
- Frequent urination or bladder pressure – Feeling like you need to go more often or having trouble emptying your bladder.
- Bowel changes – Such as constipation or diarrhea that seems related to pelvic discomfort.
- Fatigue that won’t go away – Extreme tiredness beyond normal daily life.
- Lower back pain – Persistent ache that feels connected to your pelvis.
- Bloating or abdominal swelling – A sense of fullness that doesn’t resolve.
- Painful periods – Severe cramping that’s worse than your usual experience.
These symptoms often overlap with less serious conditions, but when they persist or combine, they’re worth discussing with your doctor.

Actionable Steps You Can Take Today
Empower yourself with these practical tips to stay on top of your uterine health:
- Track your cycle – Use an app or journal to note bleeding patterns, pain levels, and any unusual discharge for at least 2-3 months.
- Schedule regular check-ups – Annual gynecological visits are key, even if you feel fine.
- Know your risk factors – Factors like obesity, diabetes, never having been pregnant, or late menopause can increase chances of issues – awareness helps you advocate for yourself.
- Don’t delay – If any sign lasts more than a few weeks, make that appointment. Early conversations with a healthcare provider often lead to simple tests like an ultrasound or biopsy for clarity.
- Adopt supportive habits – Maintain a healthy weight through balanced eating and exercise, as research links this to better hormonal balance.
These small actions can make a real difference in how quickly you get answers.

When to See a Doctor – Quick Checklist
- Any postmenopausal bleeding
- Bleeding between periods or after sex
- Persistent pelvic pain
- Unusual discharge
- Multiple symptoms together
Your body knows when something’s off – trust it and seek professional guidance.
Conclusion: Listen Before It Speaks Louder
Your uterus doesn’t have to “cry out” dramatically for you to pay attention. Those subtle, persistent signs are its way of asking for help. By recognizing them early and acting promptly, you’re taking control of your health in a powerful way. Most causes are treatable when addressed sooner rather than later. Don’t wait for things to worsen – a simple conversation with your healthcare provider could bring peace of mind or catch something early.
FAQ
What is the most common sign of endometrial concerns?
Abnormal vaginal bleeding, such as bleeding after menopause or between periods, is the most frequently reported symptom according to experts at Mayo Clinic and the American Cancer Society.
Are these symptoms always serious?
No – many have benign causes like hormonal changes or fibroids. However, any persistent or new symptom should be evaluated to rule out concerns.
How can I reduce my risk of uterine issues?
Focus on maintaining a healthy weight, staying active, and managing conditions like diabetes. Regular medical check-ups are also essential.
Disclaimer: This article is for informational purposes only and is not a substitute for professional medical advice. Always consult a qualified healthcare provider for any health concerns, diagnosis, or treatment. Early detection and personalized care are key to women’s health.
(Word count: ~1350)




