The Silent Crisis: $12$ Urgent Messages Your Uterus Is Sending You – Are You Dismissing the Call?
Imagine an essential messenger, located right at the core of your being, sending out distress signals that you routinely archive, dismiss, or simply misinterpret as “part of being a woman.” This messenger is your uterus, and its health is inextricably linked to your overall vitality, hormonal balance, and long-term well-being. For too long, the narrative around reproductive health has normalized discomfort, pain, and irregularity, leading millions of women to ignore subtle, yet critical, warnings.
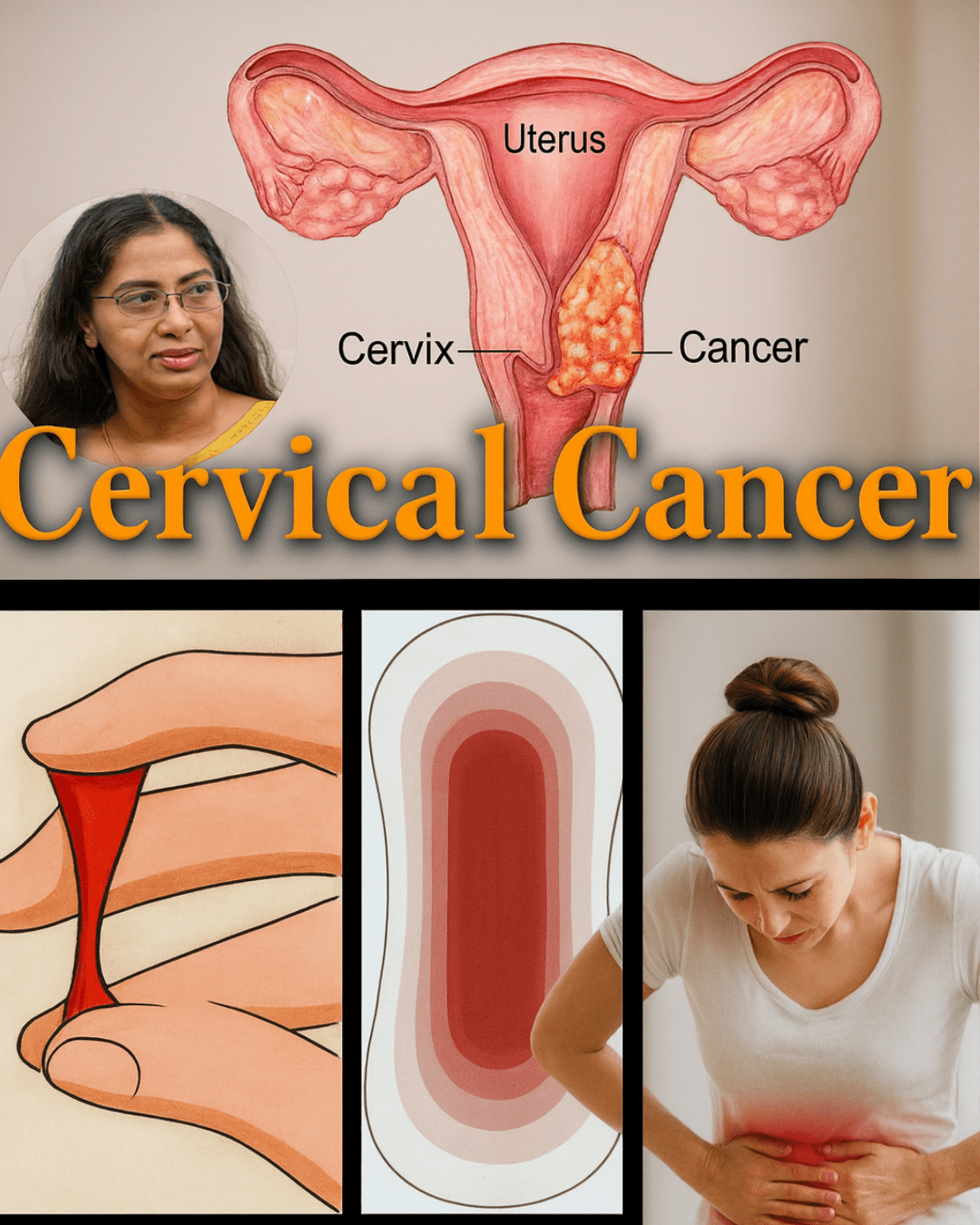
We’ve been conditioned to believe that severe menstrual cramps are just bad luck, that heavy bleeding is just “how our body is,” or that persistent pelvic discomfort is merely muscle strain. This dismissal is a dangerous misconception. The body is a meticulously designed machine, and when a core component like the uterus is struggling, it communicates through a distinct language of symptoms. Ignoring these signals doesn’t make the problem disappear; it simply allows underlying conditions like endometriosis, uterine fibroids, adenomyosis, or even early-stage cancers to advance silently and complicate treatment.
This deep-dive analysis is designed to empower you. It’s a necessary intervention against the cultural tendency to minimize women’s pain. We will meticulously unpack the $12$ most common, yet frequently overlooked, symptoms that indicate your uterus may be in urgent need of attention. Understanding these warning signs is not about inducing anxiety; it is about cultivating profound body literacy, giving you the knowledge to seek timely, decisive care, and ultimately, safeguarding your future health. Prepare to shift your perspective from passive acceptance to proactive advocacy for your own well-being.
The Foundational Crisis: Why We Fail to Listen to Uterine Signals
Before delving into the specific symptoms, it’s vital to understand the context of this issue. The uterus is a highly hormonal organ. Its function is directly tied to the complex symphony of estrogen and progesterone. When this symphony is disrupted—by stress, environmental toxins (endocrine disruptors), diet, or genetics—the uterus is often the first organ to show strain.
The Normalization Trap: The primary obstacle to early diagnosis is the cultural normalization of pain and irregularity associated with the menstrual cycle. Many women do not know the difference between a normal discomfort (mild, transient cramping) and a pathological symptom (cramps that require you to miss work or school). We need to redefine “normal” as painless, regular, and manageable. Anything outside that boundary warrants investigation.
The $12$ Critical Warning Signs: Decoding Your Uterus’s Distress Calls
These $12$ symptoms, whether experienced individually or, more commonly, in combination, form a critical checklist. If any of these resonate with your experience, it is a signal to stop, reflect, and consult a healthcare professional.
**$1$. Sudden, Persistent Irregularities in Your Menstrual Cycle
A healthy cycle is like a reliable timepiece, typically lasting between $21$ and $35$ days and remaining relatively consistent month-to-month. When this rhythm breaks down, it is a primary alarm bell. Irregularity means the cycle suddenly becomes too short (polymenorrhea), too long (oligomenorrhea), or completely unpredictable.
- Potential Culprits: Hormonal imbalances (like those seen in Polycystic Ovary Syndrome – PCOS), perimenopause, thyroid dysfunction, or structural issues like uterine fibroids or polyps that interfere with the cyclical shedding of the uterine lining.
- The Urgent Call: A missed period when you are not pregnant, or a dramatic, unexplained shift in your cycle length or flow, is the uterus signaling hormonal confusion or a physical impediment.
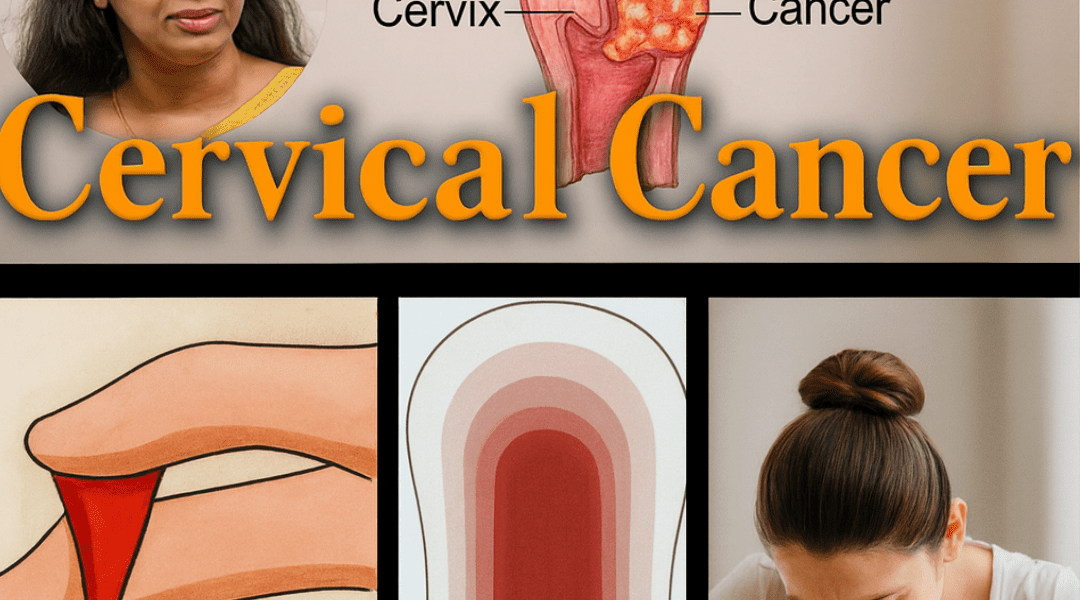
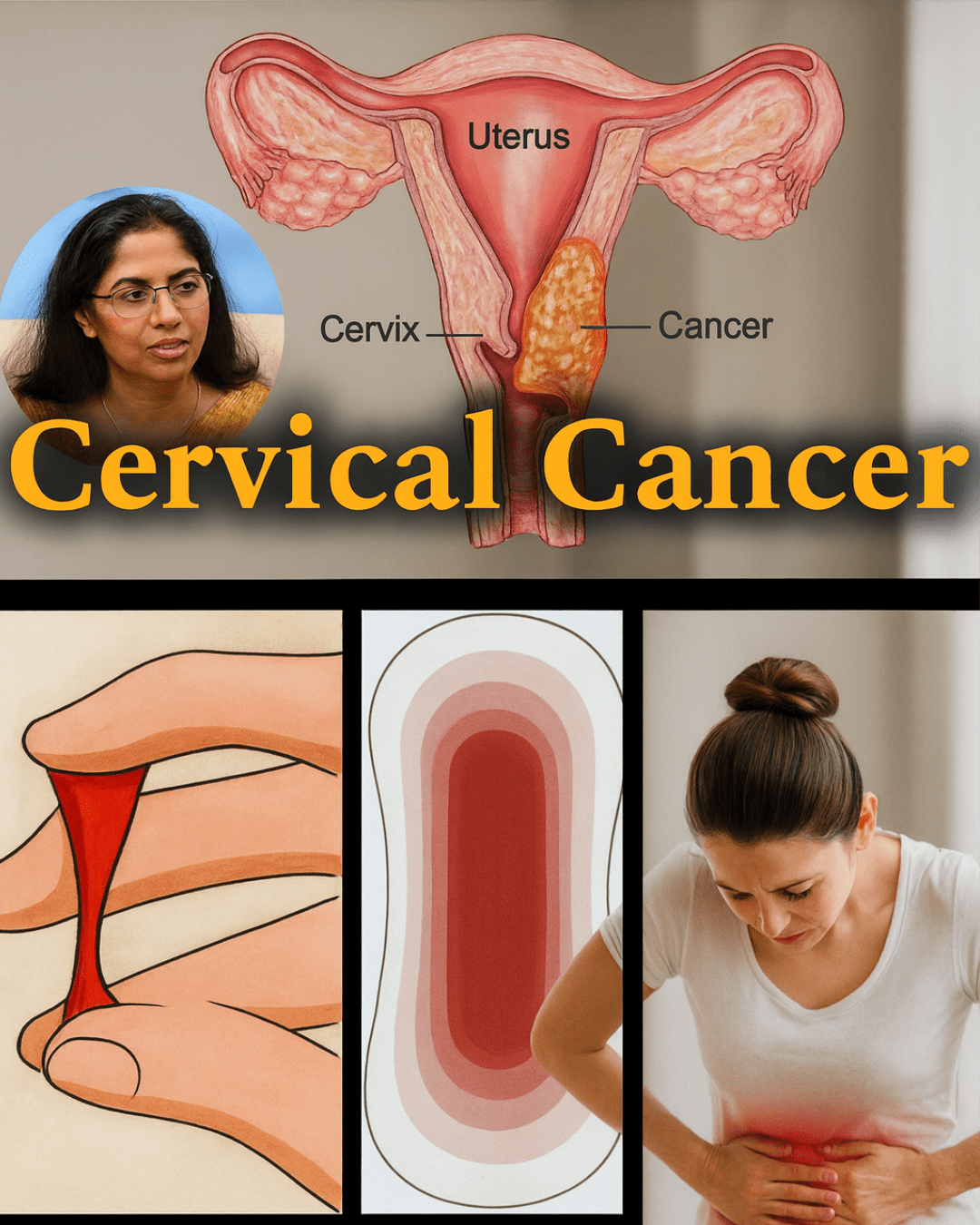
**$2$. Menstrual Bleeding Classified as Clinically Heavy (Menorrhagia)
Heavy bleeding is arguably the most dangerous symptom to ignore, primarily because of its systemic effects. Clinically heavy bleeding is defined as soaking through pads or tampons hourly for several hours, passing clots the size of a quarter or larger, or needing to double up on sanitary protection.
- Potential Culprits: The most common causes are uterine fibroids (non-cancerous tumors that grow in or on the wall of the uterus) and adenomyosis (a condition where the endometrial tissue grows into the muscular wall of the uterus). Heavy bleeding is also associated with hormonal imbalances.
- The Urgent Call: Consistent, profuse blood loss leads rapidly to iron-deficiency anemia, which manifests as profound fatigue, shortness of breath, and heart palpitations. This isn’t just a nuisance; it’s a condition that drains your life force and requires immediate correction.
**$3$. Debilitating, Life-Disrupting Menstrual Cramps (Dysmenorrhea)
Mild, tolerable cramping (primary dysmenorrhea) is common. However, cramps that force you to cancel plans, vomit, or rely heavily on prescription painkillers are not normal; they are defined as secondary dysmenorrhea, which implies an underlying pathological cause.
- Potential Culprits: Endometriosis (where tissue similar to the lining of the uterus grows outside the uterus) and adenomyosis are the two most frequent causes of agonizing period pain. Both involve inflammation and tissue growth that creates intense, often radiating, pelvic pain.
- The Urgent Call: Pain that interferes with your daily functioning is a definitive sign of inflammation or an anatomical issue that requires diagnosis and specialized treatment.
**$4$. Chronic Pelvic Pain Unrelated to Your Menstrual Cycle
The presence of persistent pain in the lower abdomen or pelvic region when you are not on your period is a significant red flag. This pain can be dull, aching, or sharp and stabbing.
- Potential Culprits: Pelvic Inflammatory Disease (PID) resulting from an untreated infection, ovarian cysts, or the deep tissue adhesion and scarring caused by long-standing endometriosis.
- The Urgent Call: Pain that lingers for more than a few days, or pain that flares up randomly, signifies a state of chronic inflammation or active infection that demands prompt medical intervention to prevent long-term damage and scarring.
**$5$. Painful Intercourse (Dyspareunia)
Discomfort, burning, or sharp, deep thrusting pain during sexual intercourse is often a difficult symptom for women to discuss, leading to avoidance and relationship strain. It is a physical symptom that is never “in your head.”
- Potential Culprits: Deep dyspareunia is frequently linked to endometriosis, where lesions are located behind the uterus or on the uterosacral ligaments. It can also indicate severe pelvic infections or uterine fibroids located near the cervix or vaginal canal.
- The Urgent Call: Painful intimacy is a clear physical manifestation of a structural or inflammatory problem that needs professional assessment, not self-blame or silent endurance.
**$6$. Abnormal Changes in Vaginal Discharge
While a slight change in the consistency of discharge is normal throughout the cycle, any sudden or extreme alterations in volume, color, consistency, or odor are direct indicators of microbial imbalance or infection.
- Potential Culprits: The most common are yeast infections, Bacterial Vaginosis (BV), or Sexually Transmitted Infections (STIs), all of which can ascend into the uterus and potentially lead to PID if left untreated.
- The Urgent Call: Discharge that becomes green, grey, chunky, foamy, or has a strong, fishy, or foul odor is the body’s warning of an active, progressing infection that must be addressed immediately to protect the upper reproductive tract.
**$7$. Frequent Urination, Urgency, or Constant Bladder Pressure
The uterus sits in close proximity to the bladder. If the uterus becomes enlarged, displaced, or develops external masses, it can press directly upon the bladder, leading to urinary distress.
- Potential Culprits: Large uterine fibroids are a leading cause. As these benign growths expand, they exert pressure, leading to the constant urge to urinate (frequency) or the feeling of incomplete bladder emptying. In rare cases, a prolapsed uterus can also place direct pressure on the bladder neck.
- The Urgent Call: Don’t assume urinary changes are solely kidney or bladder issues. If the urgency is accompanied by other pelvic symptoms, the uterus is likely the mechanical cause.
**$8$. Persistent and Unexplained Lower Back Pain
Back pain is often attributed to musculoskeletal issues—posture, lifting, or poor core strength. However, in the context of reproductive health, persistent lower back pain, especially if it intensifies during menstruation, can be a referred pain pattern originating from the pelvic cavity.
- Potential Culprits: Fibroids located on the posterior (back) wall of the uterus can press on the nerves and tissues in the lower back. Endometriosis lesions often attach to the ligaments supporting the uterus, causing chronic, radiating low back and even sciatic pain. Uterine prolapse can also cause a feeling of pelvic heaviness and lower back ache.
- The Urgent Call: If back pain is unresponsive to typical treatments (stretching, massage, rest) and fluctuates with your cycle, the source is likely gynecological, not simply orthopedic.
**$9$. Profound, Unexplained Chronic Fatigue (Beyond Normal Tiredness)
Everyone gets tired, but chronic, unshakeable fatigue that doesn’t improve with rest or sleep is a symptom that screams of a deeper physical drain. This symptom is often the first indicator of the severity of other problems.
- Potential Culprits: The most common link is iron-deficiency anemia, caused by chronic, heavy menstrual bleeding (menorrhagia) due to fibroids or adenomyosis. The constant depletion of iron and red blood cells starves the body of the oxygen needed for energy production.
- The Urgent Call: Fatigue tied to heavy periods is a literal sign that your uterus is draining your body’s essential reserves. This requires not just rest, but a diagnosis of the bleeding cause and aggressive iron supplementation.
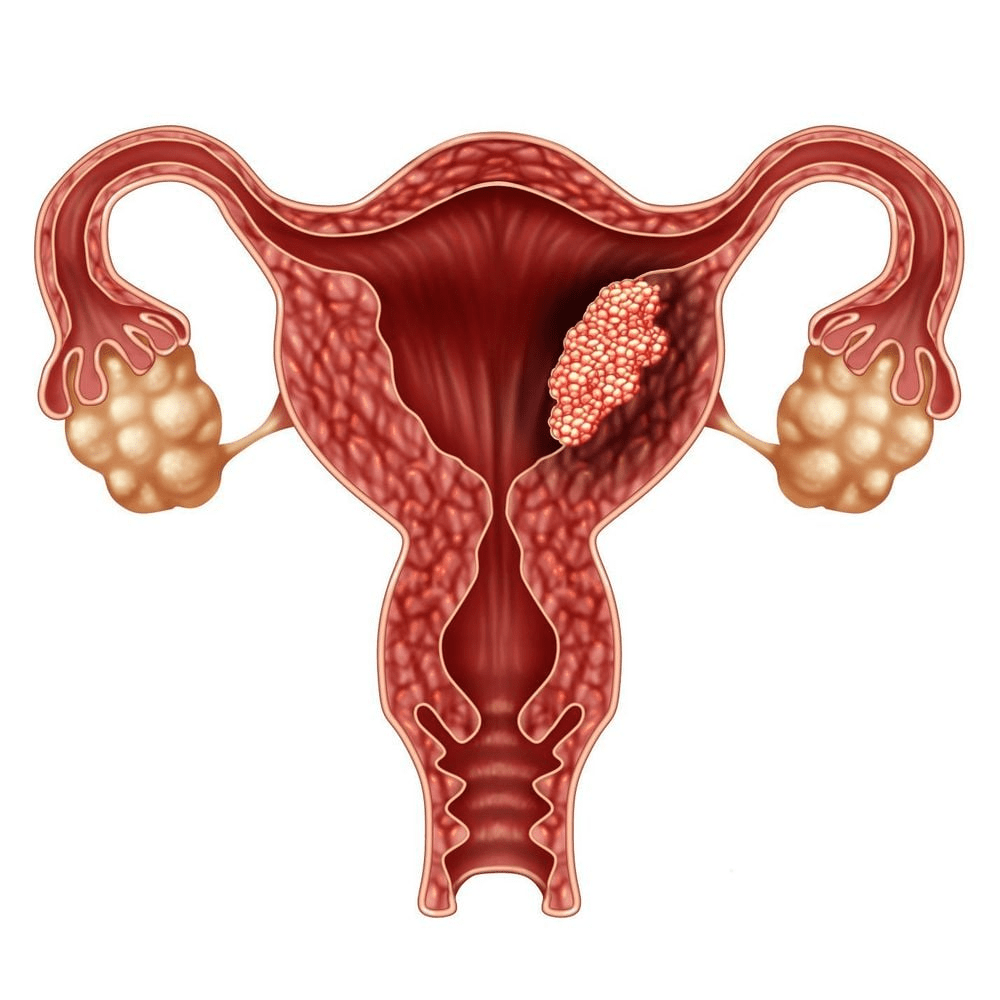
**$10$. Difficulty Conceiving or Sustaining a Pregnancy (Infertility)
While infertility has many potential causes (male factor, ovarian dysfunction), uterine issues play a major and often correctable role. The health of the uterus is paramount for implantation and gestation.
- Potential Culprits: Uterine fibroids that distort the endometrial cavity, endometrial polyps that prevent implantation, congenital structural abnormalities (like a septate uterus), or severe endometriosis that creates intense pelvic inflammation.
- The Urgent Call: If you have been trying to conceive for over a year (or six months if over $35$) and have other symptoms on this list, a thorough evaluation of the uterine cavity is a necessary first step.
**$11$. Spotting or Bleeding Between Menstrual Periods (Intermenstrual Bleeding)
Any bleeding that occurs outside of your expected menstrual window is considered abnormal and should be investigated. This symptom is particularly urgent if it occurs after menopause.
- Potential Culprits: Endometrial polyps (benign growths in the uterine lining), hormonal fluctuations often seen in perimenopause, a reaction to certain birth control methods, or, most critically, an early sign of uterine (endometrial) cancer.
- The Urgent Call: Post-menopausal bleeding is not normal under any circumstances and is considered a definitive symptom that requires immediate, rapid evaluation to rule out malignancy.
**$12$. Persistent Abdominal Bloating, Swelling, or Noticeable Abdominal Enlargement
Bloating is often blamed on diet, gas, or digestion. While sometimes true, if the feeling of constant abdominal pressure or a visible enlargement of the lower abdomen persists, the possibility of a growing mass must be considered.
- Potential Culprits: Rapidly growing or very large uterine fibroids, which can sometimes grow to the size of a grapefruit or larger. Ovarian cysts or tumors can also cause abdominal distension, mimicking digestive issues.
- The Urgent Call: If your waistline is expanding, your clothes are tight only in the lower abdomen, and you haven’t gained weight elsewhere, it is crucial to determine if a uterine or ovarian mass is responsible.
A Formula for Proactive Uterine Health: From Symptom to Solution
Understanding the $12$ warnings is the first step; the next is applying this knowledge to actionable self-care and medical advocacy. Your goal should be to move from merely observing symptoms to tracking, documenting, and demanding answers.
The Uterine Health Action Formula (The $4$ Pillars):
$1$. The Tracking Pillar (Quantification): Stop guessing. For three consecutive cycles, rigorously track:
* The Timing: The start and end date of your cycle and any spotting.
* The Intensity: Quantify bleeding (how often you change protection, clot size).
* The Pain: Rate pain on a scale of $1$ to $10$. Note when pain starts, where it radiates, and what provides relief.
$2$. The Medical Advocacy Pillar (Diagnosis): Use your documented data as evidence. Do not accept “it’s just a bad period.” Insist on specific diagnostic tools to rule out serious conditions:
* Transvaginal Ultrasound: The gold standard for visualizing the uterus, ovaries, and lining, and detecting fibroids or cysts.
* Hysteroscopy: A procedure to directly visualize the inside of the uterine cavity to find polyps or submucosal fibroids.
* Blood Tests: Check for iron and ferritin levels (for anemia) and key hormone levels (e.g., FSH, LH, Estrogen) to assess hormonal balance.
$3$. The Lifestyle Pillar (Support): Adopt habits that naturally support hormonal balance and reduce inflammation:
* Dietary Shift: Focus on anti-inflammatory foods (omega-3s, leafy greens, berries) and reduce inflammatory triggers (processed sugar, excessive refined carbs).
* Stress Management: Chronic stress elevates cortisol, which can disrupt the entire hormonal axis and worsen symptoms like endometriosis pain. Implement non-negotiable daily stress-reduction practices.
* Endocrine Disruptor Avoidance: Minimize exposure to xenoestrogens found in plastics, conventional cosmetics, and cleaning products to lessen the burden on your hormone receptors.
$4$. The Consultative Pillar (Specialization): If your symptoms are severe (e.g., suspected endometriosis or large fibroids), seek a specialist—a reproductive endocrinologist or a gynecological surgeon specializing in minimally invasive techniques. General gynecologists are excellent for routine care, but specialists often have better expertise in complex diagnoses and advanced treatments.
A Final Word on Self-Advocacy
The uterus is the cradle of creation and a barometer of feminine health. Its cry for help—whether in the form of searing pain, relentless fatigue, or a sudden change in pattern—is a crucial opportunity.
By refusing to normalize suffering and by treating these $12$ signals with the gravity they deserve, you are not just treating an organ; you are taking control of your future quality of life. Be your own most vigilant guardian. Listen to the silent crisis; your well-being depends on it.