Could Certain Habits in a Relationship Affect a Woman’s Risk of Cervical Cancer? Here’s What Research Shows
Many couples worry about how everyday choices in their relationship might impact health, especially when it comes to serious conditions like cervical cancer. This disease affects thousands of women worldwide, and while it’s often linked to a common virus, some lifestyle factors within partnerships can play a role in raising or lowering risk. Understanding these can help couples make informed decisions to protect each other.
But that’s not the whole story—there’s growing evidence pointing to specific habits that could influence outcomes, and we’ll explore them here. Keep reading to discover practical steps you can take together, including one surprising insight that many couples overlook until it’s discussed openly.
Understanding Cervical Cancer and Its Main Cause
Cervical cancer develops in the cells of the cervix, the lower part of the uterus that connects to the vagina. Nearly all cases are caused by persistent infection with high-risk types of human papillomavirus (HPV), a very common virus spread through intimate skin-to-skin contact.
Research from organizations like the World Health Organization and the American Cancer Society shows that HPV is so widespread that most sexually active people will encounter it at some point. In many cases, the body’s immune system clears the virus naturally. However, when it persists, it can lead to cell changes that may progress to cancer over time.
But HPV alone isn’t enough—other factors can make it harder for the body to fight the infection.
How a Partner’s Sexual History Can Influence Risk
One key factor highlighted in multiple studies is the number of sexual partners a person has had over their lifetime.
Studies, including those reviewed by the International Agency for Research on Cancer (IARC), have found that women whose male partners have had many previous sexual partners face a higher risk of cervical cancer. This is because a history of multiple partners increases the chances of exposure to high-risk HPV types, which can then be transmitted within the relationship.
For example:
- Research in Spain and Colombia showed that the presence of HPV on a partner’s penis significantly raised the odds for women.
- Similar findings from population studies indicate that even in monogamous relationships, past exposures can matter.
The truth is, HPV can remain dormant for years without symptoms, so it may come from experiences long before the current partnership.
This doesn’t mean blame—it’s simply about awareness. Many couples navigate this through open communication and proactive health steps.
The Role of Safe Intimacy Practices
Consistent use of barriers like condoms during intimacy can reduce (though not eliminate) the risk of HPV transmission, as the virus spreads via skin contact.
Studies suggest that habits avoiding protection, especially if one partner has unknown past exposures, may contribute to higher risk.
Here’s a quick comparison of habits that research links to HPV risk:
| Habit | Potential Impact on Risk | Supporting Insight from Studies |
|---|---|---|
| Consistent condom use | May lower transmission | Reduces exposure to HPV, per CDC guidelines |
| No barriers in high-risk scenarios | Higher chance of persistent infection | Increases skin-to-skin contact opportunities |
| Mutual monogamy with testing | Generally lower | Limits new exposures |
But that’s not all—another common habit in relationships can add to the challenge.
Smoking and Secondhand Exposure: An Often Overlooked Factor
Smoking is a well-established risk factor for many cancers, including cervical.
Chemicals in tobacco can damage cervical cells and weaken the immune response to HPV. Even secondhand smoke exposure has been linked in some studies to increased risk.
Research, including cohort studies, shows:
- Women exposed to regular secondhand smoke may have elevated odds.
- Partners who smoke could indirectly affect this through shared environments.
Quitting together or creating smoke-free spaces can make a real difference.
Here are evidence-based ways to reduce this risk:
- Avoid smoking entirely.
- Limit exposure to secondhand smoke at home.
- Support each other in cessation programs—studies show couples quit more successfully together.
This brings us to the part many find most helpful: what you can do right now.

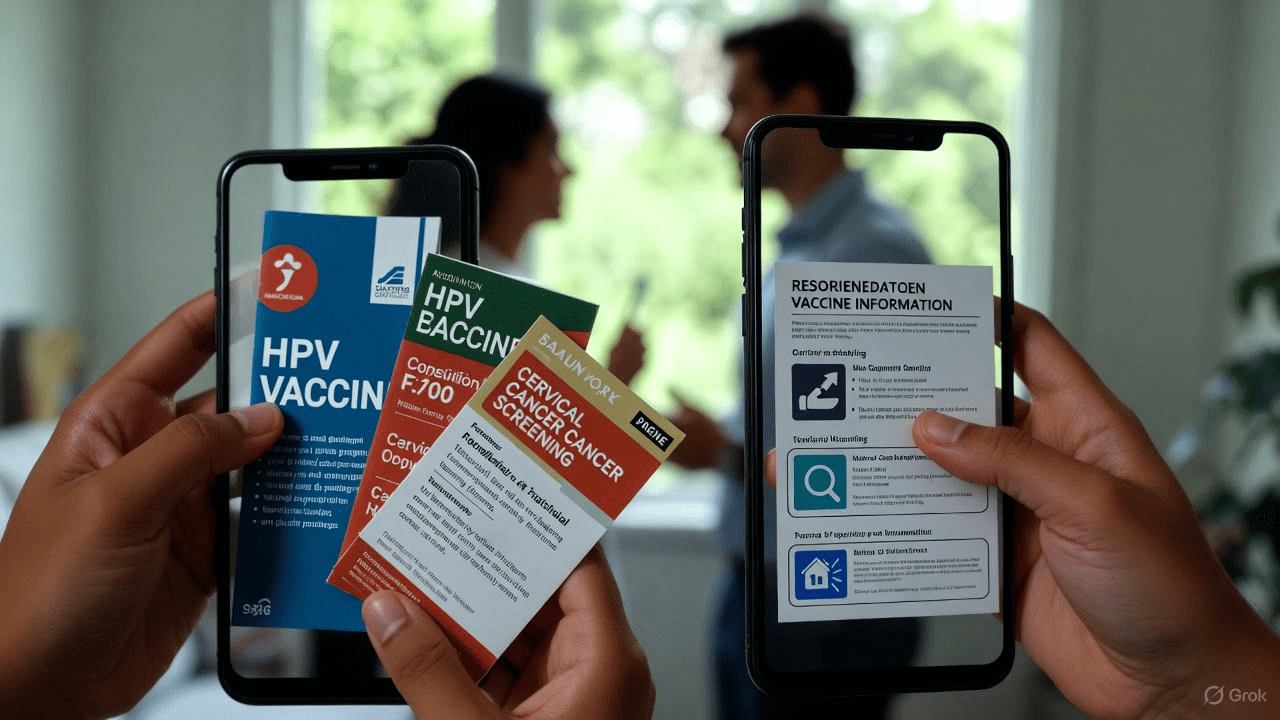
Actionable Steps Couples Can Take to Lower Risk
Protecting health in a relationship is a team effort. Here are practical, step-by-step tips based on guidelines from major health organizations:
- Get vaccinated: The HPV vaccine is highly effective against the most common high-risk types. It’s recommended for both men and women up to age 45 in many cases—talk to your doctor.
- Prioritize regular screening: Women should follow Pap and HPV testing schedules. Early detection changes everything.
- Practice safer intimacy: Use barriers consistently, especially early in relationships or if concerns arise.
- Maintain good hygiene: Daily gentle cleaning supports overall genital health and may help the body manage infections.
- Avoid tobacco: Quit smoking and minimize secondhand exposure for better immune function.
- Communicate openly: Discuss sexual histories and testing without judgment—it strengthens trust and health.
These steps aren’t about fear; they’re empowering choices that research shows can significantly reduce risks.
In Conclusion: Empowering Choices for Healthier Relationships
Cervical cancer is largely preventable with awareness, vaccination, screening, and healthy habits. While HPV is the primary driver, factors like past sexual histories, intimacy practices, and tobacco exposure can influence outcomes in partnerships.
By focusing on mutual support—vaccination, open talks, safer choices, and regular check-ups—couples can greatly lower risks and enjoy peace of mind.
The surprising insight? Many studies emphasize that male vaccination and habits benefit women too, creating a shared protective effect.
Frequently Asked Questions (FAQ)
1. Can cervical cancer be completely prevented?
While no prevention is 100% guaranteed, HPV vaccination, regular screening, and healthy lifestyle choices prevent the vast majority of cases, according to major health bodies.
2. Does having only one partner eliminate the risk?
Monogamy reduces new exposures, but past infections can persist. Screening remains important regardless of relationship status.
3. Should men get the HPV vaccine too?
Yes—vaccinating men protects them from HPV-related issues and reduces transmission to partners, as supported by health guidelines.
Disclaimer: This article is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare provider for personalized guidance on health concerns.